Tiểu đường là căn bệnh mạn tính ảnh hưởng đến hàng triệu người. Tuy nhiên, gánh nặng của bệnh tiểu đường không được phân bổ đồng đều cho tất cả các cộng đồng. Một số nhóm người nhất định, chẳng hạn như người Mỹ bản địa, người da màu, người gốc Tây Ban Nha và người châu Á, phải đối mặt với những rủi ro và kết quả khác nhau, vì thế thiết kế các chiến lược quản lý và dự phòng cho những nhóm người này sao cho có thể phù hợp nhất về phương diện văn hóa trở nên rất cấp bách.
Tại sao nguy cơ mắc bệnh tiểu đường và tỷ lệ tử vong lại khác nhau giữa các nhóm dân tộc
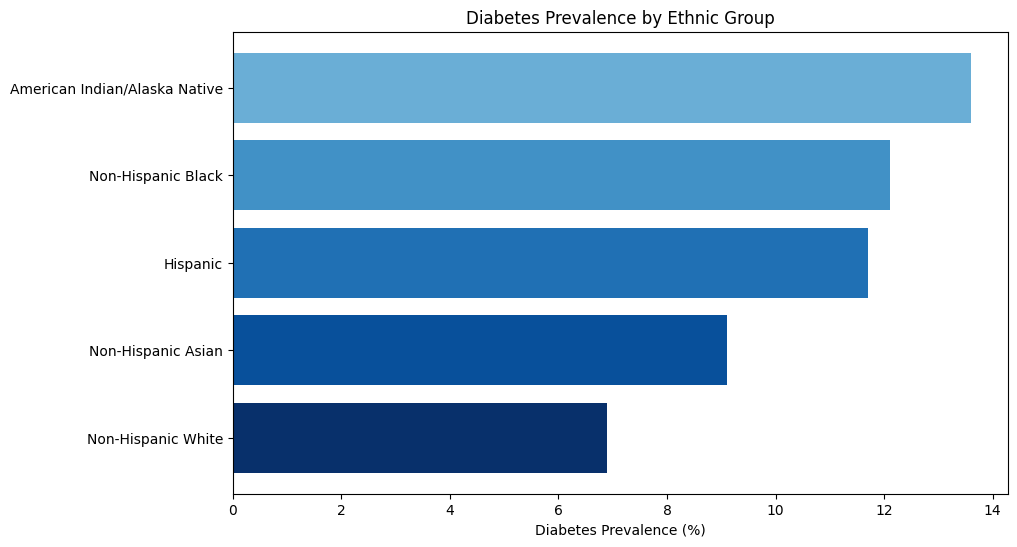
Tỷ lệ mắc bệnh tiểu đường cao nhất ở người Mỹ bản địa, với 13.6% trong nhóm này được chẩn đoán mắc bệnh. Theo sau họ là người da màu trưởng thành không phải gốc Tây Ban Nha (12.1%) và người trưởng thành gốc Tây Ban Nha (11.7%). Người trưởng thành gốc Á không phải gốc Tây Ban Nha có tỷ lệ mắc bệnh là 9.1%, mặc dù thấp hơn các nhóm trên nhưng vẫn cao hơn đáng kể so với người trưởng thành da trắng không phải gốc Tây Ban Nha, có tỷ lệ mắc bệnh là 6.9%. Những khác biệt này nhấn mạnh sự ảnh hưởng của các yếu tố như di truyền, lối sống và kinh tế xã hội đến nguy cơ mắc bệnh tiểu đường.
Nguồn: Viện nghiên cứu Quốc gia về bệnh đái tháo đường, bệnh tiêu hóa và thận. “Thống kê về bệnh tiểu đường.” Truy cập tại https://www.niddk.nih.gov/health-information/health-statistics/diabetes-statistics.
Những sự cân nhắc đặc biệt: BMI và nguy cơ mắc bệnh tiểu đường ở các dân tộc
Chỉ số khối cơ thể (Body Mass Index - BMI) là một yếu tố quan trọng trong việc đánh giá nguy cơ mắc bệnh tiểu đường, nhưng việc áp dụng tiêu chuẩn của nó có thể gây nhầm lẫn giữa các nhóm dân tộc khác nhau:
• Người Mỹ gốc Á và ngưỡng BMI thấp hơn: Người Mỹ gốc Á có xu hướng phát triển bệnh tiểu đường loại 2 ở mức BMI thấp hơn so với các nhóm khác. Do sự khác biệt về thành phần cơ thể, bao gồm xu hướng béo bụng cao hơn, Hiệp hội Đái tháo đường Hoa Kỳ (American Diabetes Association - ADA) khuyến cáo người Mỹ gốc Á nên sàng lọc bệnh tiểu đường khi chỉ số BMI của họ từ 23 trở lên, so với ngưỡng tiêu chuẩn là 25. Sự điều chỉnh này thừa nhận rằng ngay cả ở mức độ được coi là chỉ số BMI “bình thường”, người châu Á có thể có nguy cơ mắc bệnh tiểu đường cao hơn do các yếu tố như tích tụ mỡ nội tạng.
Trong những năm gần đây, CDC và Viện Y tế Quốc gia (National Institute of Health) đã công nhận rằng người Mỹ gốc Á có thể có nguy cơ mắc hoặc phát triển bệnh tiểu đường theo những cách khác biệt với các nhóm người khác. Điều này có nghĩa là, mặc dù bạn có thể ăn những món mà những người xung quanh có vẻ dùng được ổn nhưng bạn có thể cần phải thận trọng hơn về cân nặng của mình, ngay cả khi bạn trông khỏe mạnh khi so sánh với những người hàng xóm của mình.
• Tiêu chuẩn BMI ở các nhóm người Mỹ bản địa, người da màu và gốc Tây Ban Nha: Ngưỡng BMI tiêu chuẩn (trên 25 là thừa cân, trên 30 là béo phì) áp dụng cho hầu hết các nhóm dân cư, bao gồm các nhóm người Mỹ bản địa, da màu và gốc Tây Ban Nha. Tuy nhiên, tỷ lệ béo phì cao hơn trong các cộng đồng này góp phần đáng kể vào việc gia tăng tỷ lệ mắc bệnh tiểu đường loại 2. Béo phì có liên quan chặt chẽ đến tình trạng đề kháng insulin, đây là nguyên nhân chính thúc đẩy sự phát triển của bệnh tiểu đường loại 2. Các sáng kiến y tế công cộng ở những cộng đồng này thường tập trung vào việc quản lý cân nặng, tăng cường hoạt động thể chất và cải thiện khả năng tiếp cận những thực phẩm lành mạnh để giảm nguy cơ mắc bệnh tiểu đường.
Chiến lược phòng ngừa có mục tiêu cho các cộng đồng nguy cơ cao
Giảm nguy cơ mắc bệnh tiểu đường đòi hỏi sự kết hợp giữa thay đổi lối sống cá nhân và sự trợ giúp của toàn cộng đồng. Dưới đây là những chiến lược hiệu quả, đặc biệt quan trọng đối với những người thuộc các nhóm dân tộc có nguy cơ cao:
• Phương pháp ăn uống cân bằng phản ánh sở thích văn hóa: Bữa ăn nhiều rau, thịt nạc, ngũ cốc nguyên hạt và chất xơ có thể điều chỉnh lượng đường trong máu. Lời khuyên về cách thức ăn uống phù hợp với văn hóa có thể giúp các cá nhân đưa ra những lựa chọn lành mạnh hơn phù hợp với các thực phẩm truyền thống, giảm tiêu thụ các loại thực phẩm đã qua chế biến và có đường.
• Khuyến khích hoạt động thể chất trong môi trường cộng đồng: Hoạt động thể chất thường xuyên là cần thiết, nhưng việc kết hợp các hình thức tập thể dục được ưa chuộng về mặt văn hóa, chẳng hạn như khiêu vũ theo nhóm hoặc thể thao cộng đồng, có thể làm gia tăng sự tham gia. Để có kết quả tối ưu, hãy đặt mục tiêu 150 phút hoạt động vừa phải hàng tuần.
• Chương trình quản lý cân nặng có mục tiêu: Duy trì cân nặng khỏe mạnh giúp làm giảm đáng kể nguy cơ mắc bệnh tiểu đường. Các chương trình được thiết kế phù hợp với dân tộc, có tính đến phong tục ăn uống và sự tiếp cận các loại thực phẩm cụ thể, có thể giúp việc quản lý cân nặng trở nên khả thi và bền vững hơn.
• Khám sàng lọc định kỳ cho các nhóm có nguy cơ: Sàng lọc sớm có thể xác định tình trạng tiền tiểu đường, cho phép thực hiện các biện pháp can thiệp nhằm ngăn chặn sự tiến triển. Các trung tâm y tế cộng đồng và các sáng kiến giáo dục sức khỏe phù hợp với văn hóa đóng một vai trò quan trọng trong việc bảo đảm các hoạt động sàng lọc này có thể thực hiện được.
Phương pháp tiếp cận toàn diện để quản lý bệnh tiểu đường
Đối với những người đã được chẩn đoán mắc bệnh tiểu đường, việc quản lý hiệu quả sẽ giúp làm giảm các biến chứng và cải thiện chất lượng cuộc sống:
• Cá nhân hóa việc theo dõi đường huyết: Việc theo dõi thường xuyên cho phép các cá nhân thực hiện các điều chỉnh về phương pháp ăn uống và lối sống một cách sáng suốt. Các chương trình và phòng khám cộng đồng dễ tiếp cận có thể trợ giúp những nỗ lực này, đặc biệt là ở những khu vực chưa được quan tâm đúng mức.
• Tuân thủ dùng thuốc: Việc tuân thủ các loại thuốc được kê đơn và liệu pháp insulin là điều cần thiết. Trợ giúp các chuyên gia chăm sóc sức khỏe có hiểu biết về văn hóa có thể cải thiện sự tuân thủ và tạo dựng niềm tin ở bệnh nhân.
• Giáo dục về dinh dưỡng qua lăng kính văn hóa: Nhấn mạnh vào các thực phẩm có chỉ số đường huyết thấp phù hợp với các bữa ăn truyền thống giúp kiểm soát lượng đường trong máu mà không làm thay đổi mạnh mẽ thói quen ăn uống. Các loại thực phẩm như rau lá xanh, thịt nạc và ngũ cốc nguyên hạt giúp ổn định lượng đường trong máu cũng như ngăn ngừa sự gia tăng đường huyết đột ngột.
• Sự tham gia của cộng đồng vào hoạt động thể chất: Duy trì hoạt động thể chất là rất quan trọng trong việc quản lý bệnh tiểu đường. Các chương trình tập thể dục dựa vào cộng đồng mang tính văn hóa có thể giúp các cá nhân tham gia vào hoạt động thể chất một cách thường xuyên.
Tiến tới phòng ngừa và quản lý bệnh tiểu đường một cách toàn diện
Tỷ lệ mắc bệnh tiểu đường cao hơn ở một số cộng đồng nhất định đòi hỏi những cách tiếp cận nhạy cảm về văn hóa. Nhân Ngày Đái tháo đường Thế giới, chúng ta hãy ưu tiên các nguồn lực chăm sóc sức khỏe dễ tiếp cận, tập trung vào cộng đồng, phục vụ nhu cầu đặc biệt của những nhóm dân số có nguy cơ cao. Bằng cách kết hợp các biện pháp can thiệp y tế công cộng có mục tiêu, biện pháp chăm sóc có nhận thức về văn hóa và các chính sách trợ giúp, chúng ta có thể giúp làm giảm các biến chứng liên quan đến bệnh tiểu đường và cải thiện kết quả sức khỏe ở những cộng đồng khác nhau.
Hãy cam kết hướng tới một tương lai nơi mọi người đều được tiếp cận dịch vụ chăm sóc sức khỏe được thiết kế riêng, phù hợp về phương diện văn hóa để giúp có được một cuộc sống khỏe mạnh hơn, với bất kể nguồn gốc nào. Việc nhận được thông tin đầy đủ có thể giúp bạn thực hiện các bước chủ động để ngăn ngừa và quản lý căn bệnh này. Trung Tâm Y Khoa Phương Bắc (Northern Medical Center) luôn sẵn sàng trợ giúp bạn. Hãy gọi đến số 845 800 5118 hoặc đặt lịch hẹn trực tuyến để được tư vấn.
Nguồn tham khảo
“Diabetes Statistics,” National Institute of Diabetes and Digestive and Kidney Diseases, U.S. Department of Health and Human Services.
“Diabetes and Racial and Ethnic Minority Groups,” Centers for Disease Control and Prevention.
“Diabetes and Asian Americans,” U.S. Department of Health and Human Services, Office of Minority Health.
“Understanding Risk: Asian Americans and Diabetes,” Diatribe Foundation.